Adenomyosis
Adenomyosis is diagnosed when endometrial glands and stroma invade 2-3 mm into the uterine muscle (1-2 high power fields below the endometrium). Bleeding and collection of blood into the muscle during menstrual time leads to local inflammation and scar tissue formation causing hypertrophy and hyperplasia of the myometrium. It is more common in women over the age of 40 years who account for 80% of all cases. However it is more associated with the following:
- Previous repeated childbirth as 80% of all cases are parous women.
- After intrauterine operations including D&C and evacuation of the uterus.
- Some reports associate adenomyosis with previous caesarean section and tubal ligation.
A common factor to most these causes is the breakdown in the normal endometrial / myometrial interface which could allow migration of endometrial glands and stroma into the adjacent muscle.
There is 80% chance of another pelvic pathology mainly fibroids in 50%, endometriosis in 11% and endometrial polyps in 7% of the cases.
Presentation
- Pelvic pain
- painful menstruation
- Heavy periods
- Painful intercourse
- Infertility
In almost 50% of cases there are no related symptoms and it is only a chance finding. It is more likely that symptoms occur with deeper penetration and wider distribution of the pathology.
Types of adenomyosis
Diffuse lesions occupy a wide area of the uterine muscle. It could show as:
 |
| Oblique view of a uterus showing posterior wall subendometrial adenomyotic focal areas with similar echogenicity as the neighbouring endometrium and a large vaguely circumscribed disharmonious adenomyoma with hypoechoic cysts occupying most of the posterior uterine wall. Harmonic imaging was used in this case to magnify the different texture shown by the adenomyotic lesions |
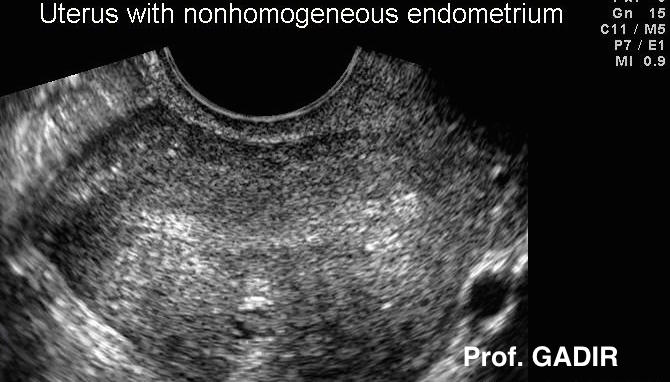
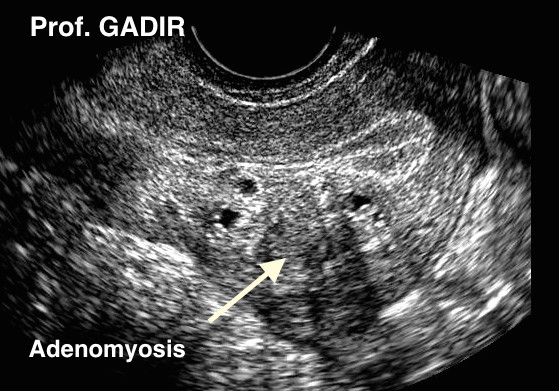
- Non homogenous myometrium in a patient who presented
- with heavy menstruation, severe dysmenorrhoea and
- dyspareunia. The scan was done during the very early
- follicular phase
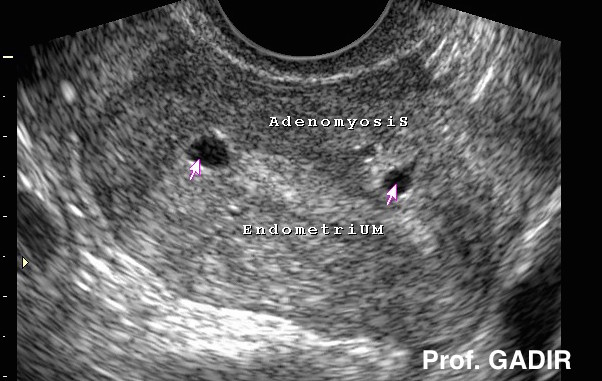
This luteal phase ultrasound image shows the same uterus
depicted in the picture above. It showed subendometrial
focal adenomyotic lesions connected to the endometrial line.
These lesions can be removed easily with the restectoscope
The message here is to repeat the ultrasound scan
examination during the late luteal phase if there is any
diagnostic doubt, or MRI is not immediately available.
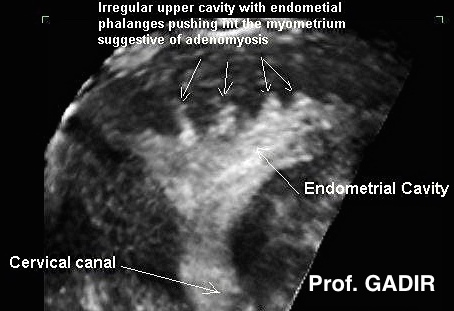
Coronal view of a uterus showing adenomyotic projections
into the fundal myometrium. The patient had severe
dysmenorrhoea and excessive menstrual loss. 2D scanning
was not as diagnostic as 3D in this case. Yet again,
performing the scan during the luteal phase allowed the
echogenic projections to stand out against the hypoechoic
myometrium.

- Occasionally, subendometrial adenomyosis may be so severe
- that diagnosis can be made easily at any stage of the cycle.
- This is especially so if multiple cystic areas are seen around
- an indiscriminate endometrial line, as demonstrated by the
- neighbouring ultrasound image.
Focal lesions are localised to one or two areas mostly subendometrial or alternatively as difficulty in clear identification of the endometrium / myometrium interface by transvaginal scan examination
Occasionally colour Doppler studies can give some help in differentiating between fibroids and adenomyotic areas. Fibroids usually show peripheral vasculature as seen in the first image below with colour Doppler mapping, where as the adenomyotic area in second image showed through vascularisation.
Diagnosis
The uterus is usually enlarged but regular in shape. It could be tender during bimanual vaginal examination.
Previously histological examination of hysterectomy specimens was the only means for diagnosing adenomyosis. However recently both MRI and transvaginal scan examinations are used for the pre-surgical diagnosis of the disease.
MRI is very sensitive in showing widening of the junctional zone but transvaginal scan examination is also 80% sensitive in diagnosing adenomyosis. Moreover transvaginal scanning facilitates needle biopsy and histological examination of suspected areas.
Though adenomyotic glands are not fully responsive to progesterone, yet transvaginal scan examinations during the luteal phase is more likely to give a better illustration of subendometrial focal lesions in my experience.
On the other hand hysteroscopy is not very useful in establishing the diagnosis in most cases. A hysteroscopically directed single biopsy is less than 20% sensitive in diagnosing adenomyosis. However it has 100% specificity when the correct area has been biopsied. The low sensitivity can be improved by using transvaginal scan directed biopsies.
Deep diffuse lesions are not accessible hysteroscopically but subendometrial lesions may occasionally show in different ways. Reducing intrauterine pressure during endometrial resection may allow the adenomyotic lesions to hang down as dark or black projections into the uterine cavity after excision of the superficial area overly lying the lesions.
- The first hysteroscopic image above shows landmarks within the uterine cavity; 1 - 4 depict adenomyotic lesions while 5 depicts the ostium of the left tube.
- The second image shows the same uterine cavity after excision of the superficial area over point 1. This revealed adenomyotic tissue hanging into the cavity, after reducing the pressure.
Management
As up to 50% of patients with adenomyosis are not symptomatic treatment should not be offered on incidental ultrasonic diagnosis. It should depend on the presenting symptom whether it is pain, menorrhagia or infertility. Medical treatment is usually directed towards controlling pain and abnormal uterine bleeding with:
On the other hand surgical treatment is used in certain cases when medical treatment proved unsuccessful. It could be conservative or definitive in nature. The modalities used include:
Hysteroscopic local resection after treatment with GnRH-a could be effective for subendometrial focal lesions presenting with excessive bleeding. However it is only 50% effective in controlling pain.
Hysterectomy could be offered as a definitive treatment for patients who completed their families. However no studies have yet been done to show how effective this treatment is in resolving pelvic pain. An estimate of 80% has been suggested as pelvic pain is usually multifactorial.
Recent reports showed a place for uterine artery embolisation in the treatment of adenomyosis in women not willing to accept definitive surgery.
The above 2 images show 2 areas of histologically confirmed subendometrial adenomyosis before and after hysteroscopic excision with a resectoscope.
The hysteroscopic picture above shows an area of subendometrial adenomyosis within the muscle during resection. Note the many tubular structures and hollow spaces within the muscle in this patient. She presented with menorrhagia and dysmenorrhoea. Histopathological assessment confirmed the presence of adenomyosis



